Precision automation
for specialty drugs
Mandolin replaces fragmented workflows with AI agents that execute the end-to-end lifecycle, including intake, benefits, prior authorizations, and revenue cycle management. Increase throughput without increasing headcount.
.svg)
.svg)
.svg)
.svg)
Scale profitability while improving quality of care
Increase speed, increased revenue
Faster benefits checks and authorizations lead to more completed treatments, quicker payments, and stronger top-line growth.
Reduce bad debt and overhead
Automated accuracy ensures coverage is verified and payments are collected — cutting manual work and preventing revenue leakage.
Elevate patient experience
Faster intake and approvals means that patients have clearer expectations and fewer delays.
Back office full of your best employee
AI models now perform the labor historically found in a back office: Navigating systems, reading faxes, making phone calls, and reasoning with data. Mandolin is the first and only company designed from the ground up to cover the end-to-end back office tasks for administering specialty drugs.
Our results speak for themselves
Mandolin helps infusion centers accelerate authorizations, reduce denials, and unlock more revenue — all without adding staff. Explore real-world case studies showing how clinics are scaling profitably while improving patient access and experience.
Workflows, not widgets
No APIs. No integrations. Every step, fully automated.
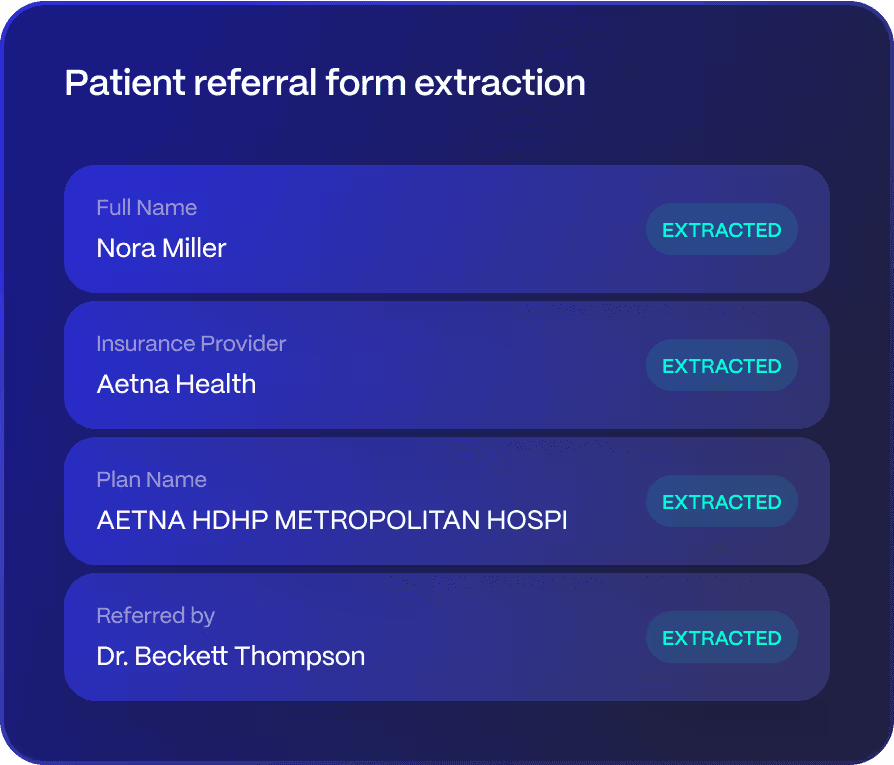
Intake & Onboarding
Mandolin instantly reads, interprets, and acts on referral forms, lab reports, and clinical notes — regardless of formatting or source and enters it into your EHR.
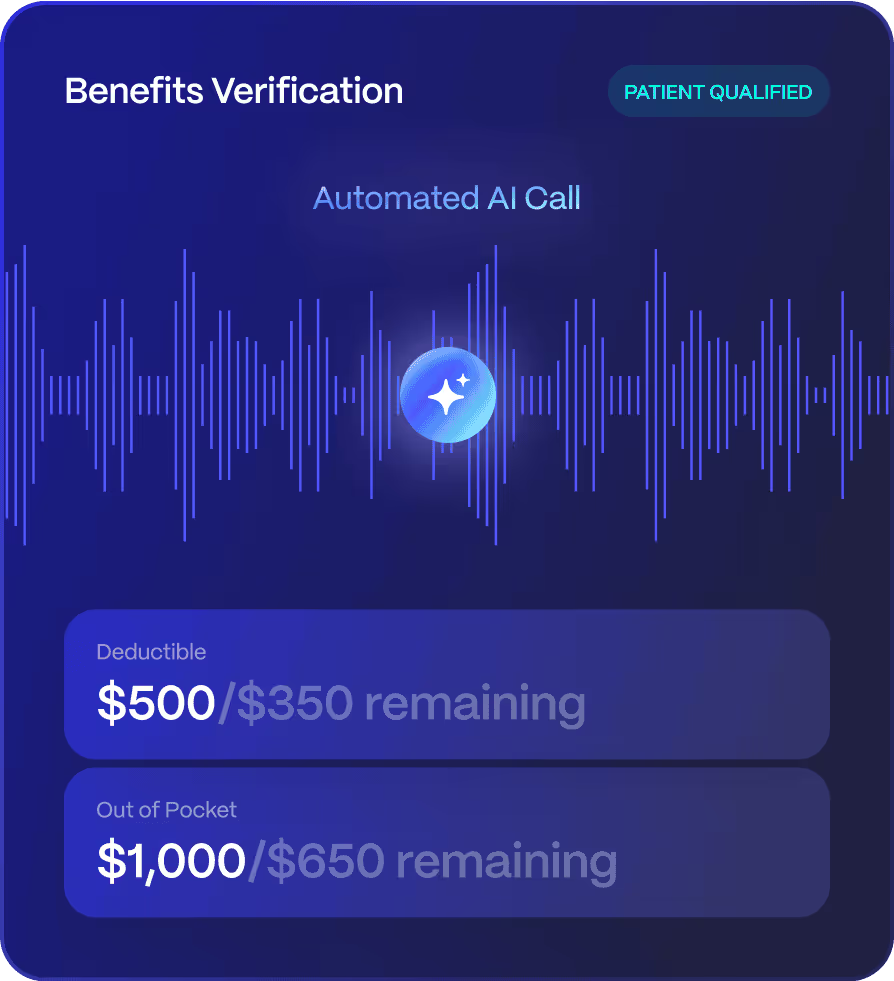
Benefits Verification
Mandolin performs full benefits investigations by navigating payer portals, extracting eligibility data, and making outbound calls — just like a trained back-office specialist.
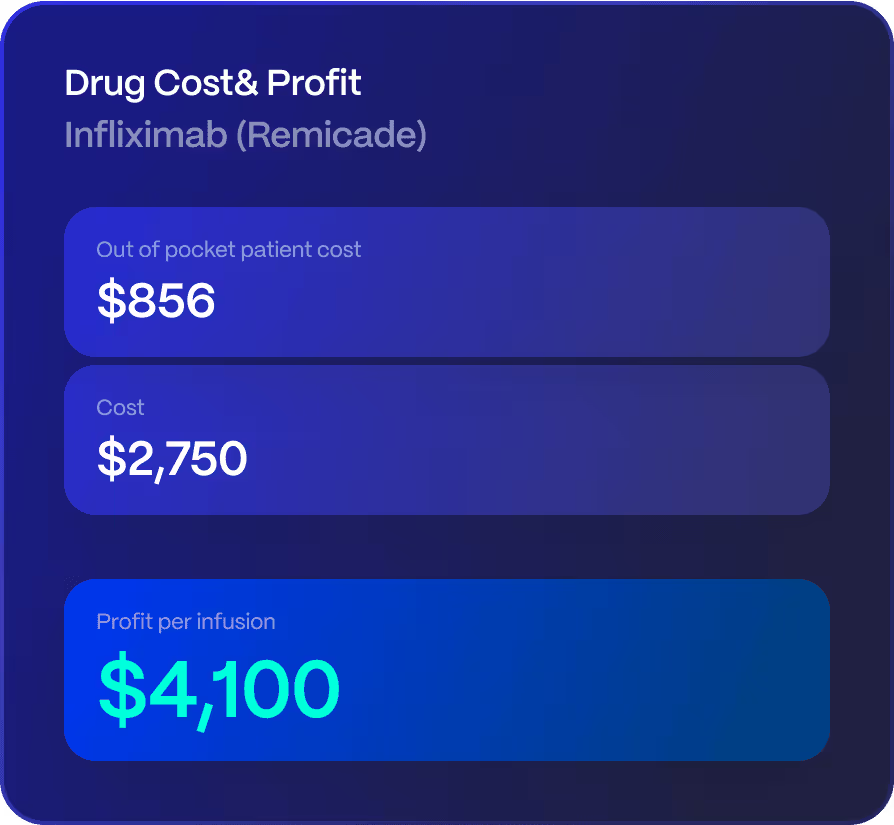
Patient Out-Of-Pocket Estimation
Calculates patient out-of-pocket costs with precision — factoring in real-time benefits, site-specific fee schedules, co-pay assistance, GPO and 340B pricing, and drug acquisition costs.
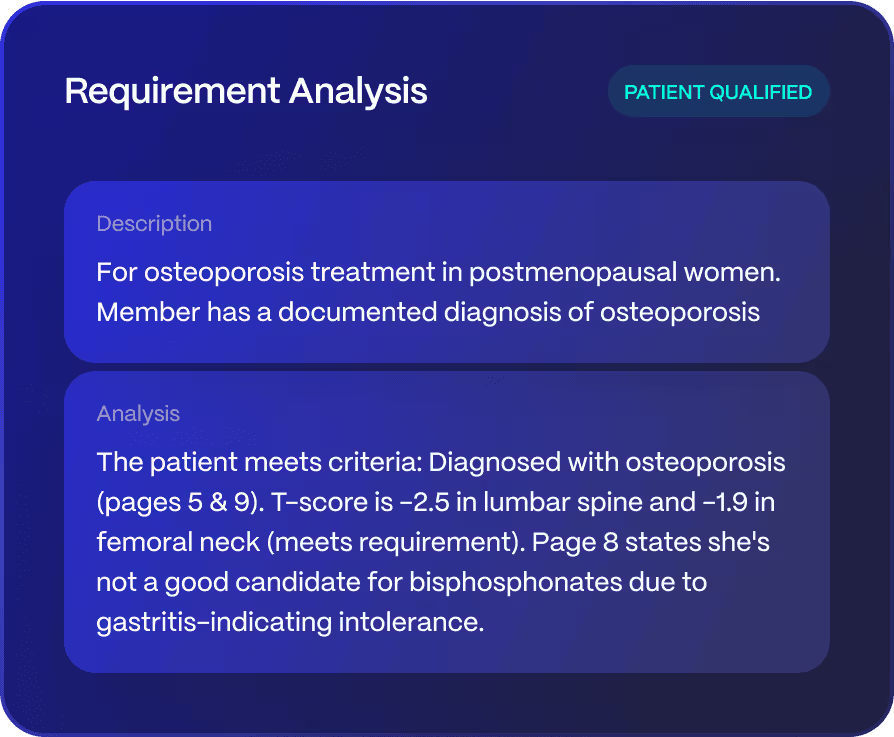
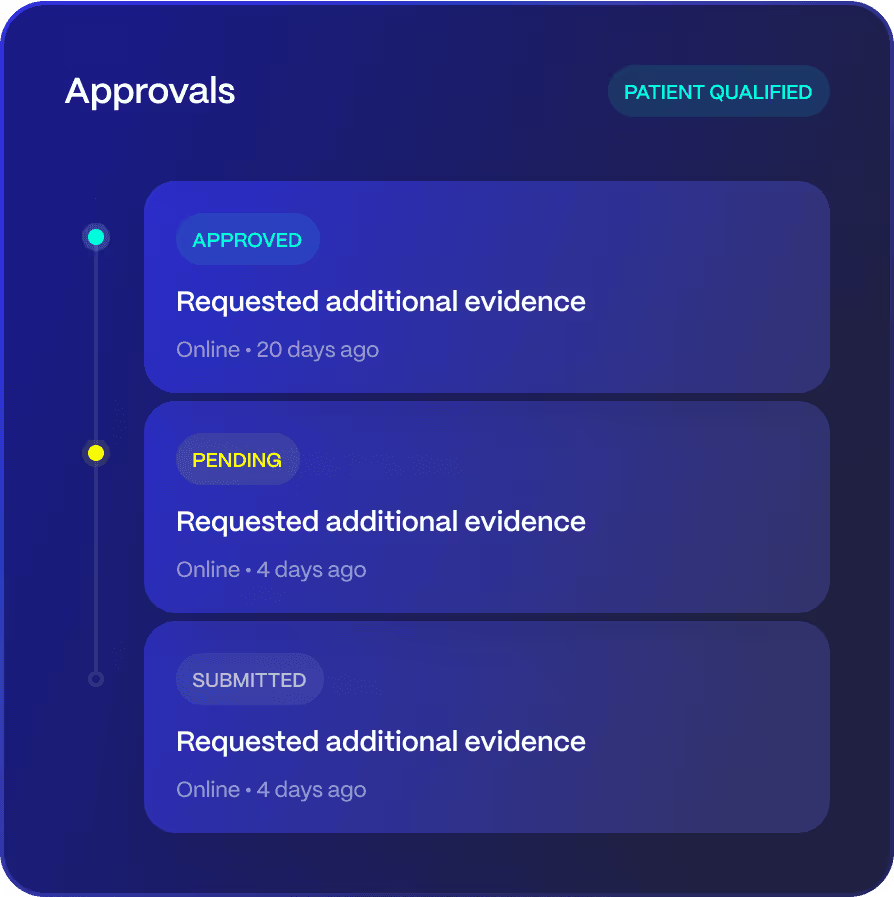
Medical Policy Review & Prior Authorization
Compares medical policy requirements with patient charts then compiles and submits prior auths via portals, faxes and phone calls.
Claims Statusing and Appeal Automation
Tracks claim status automatically by making portal checks or payer calls then interpreting remits so your team doesn’t spend hours chasing for updates.
Fully Compliant,
Always Transparent
Mandolin is built with compliance at its core — every action our AI agents take is logged, traceable, and aligned with payer requirements and healthcare regulations.


Let’s talk
We'll be in touch within 24 hours.



